Alzheimer’s disease is one of the most devastating conditions. My Grandad suffered from the disease and it was heartbreaking to witness.
However, Alzheimer’s is NOT part of the natural ageing process.
While it can’t be cured at this moment in time, modern research is teaching us lots about how the disease develops and, therefore, how it can be prevented.
Unfortunately, you probably won’t get much useful advice regarding preventative measures from your doctor.
This is because they are incentivised to push profitable pharmaceutical drugs over free lifestyle interventions.
But there are a lot of great researchers out there sharing their findings and offering novel solutions to the problem of dementia and Alzheimer’s (Alzheimer’s is a type of dementia).
This article will explain what we currently know about Alzheimer’s disease, including recent developments on its cause and how it may be prevented.
What is Alzheimer’s disease?
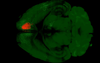
Alzheimer's disease is a progressive and degenerative neurological disorder that primarily affects the brain, leading to cognitive decline, memory loss, and a range of other cognitive and behavioural symptoms.
It is the most common cause of dementia among older adults.
The disease is characterised by the gradual accumulation of abnormal protein deposits in the brain, particularly beta-amyloid plaques and tau tangles.

These deposits interfere with the normal functioning of brain cells, leading to their damage and eventual death.
As brain cells are lost, individuals with Alzheimer's experience a decline in cognitive abilities, including memory, language, problem-solving skills, and the ability to perform everyday tasks.
The symptoms of Alzheimer's disease typically progress from mild memory problems to severe impairment, affecting an individual's quality of life and their ability to carry out basic activities.
In the later stages, individuals may become disoriented, have difficulty recognising loved ones, and may experience personality changes.
Alzheimer's disease has no known cure, and it is a leading cause of disability and dependency in the elderly population.
It is a condition that affects not only the individuals diagnosed but also places a significant emotional and practical burden on their caregivers and families.
Treatment for Alzheimer's primarily focuses on managing symptoms and providing support to enhance the quality of life for those affected.
Outdated theories of Alzheimer’s
There is a long-standing belief that Alzheimer's is caused by the accumulation of beta-amyloid protein.
However, despite decades of investigation and numerous clinical trials targeted at reducing or preventing beta-amyloid build up, no successful treatments have emerged.
In 2021, it was also revealed that data in influential papers had been faked, which has cast further doubt on the hypothesis.
In simple terms, creating a drug to reverse, stop or even slow down Alzheimer's disease has been fruitless.
It's true that amyloid plays a role in the brain and dementia, but Alzheimer's disease is complicated and there's much more to it than just one molecule.
We've been targeting the mediators instead of the root causes (e.g. toxins, inflammation and insulin resistance). We need to look at other ideas to find a cure.
New findings: the gut microbiota and Alzheimer’s
A recent study has found the gut microbiome plays a vital role in the development of Alzheimer's.
Using gut microbiota transplants, a research team has demonstrated that memory impairments observed in individuals with Alzheimer's can be transmitted to young, healthy rats.
The study found that the rats who received microbiota from Alzheimer's patients exhibited impaired memory behaviours, particularly those associated with a process known as adult hippocampal neurogenesis.
This process generates new neurons in the hippocampus, a crucial brain region for memory and mood, and one of the earliest areas affected by Alzheimer's disease.
The study also found that one specific strain of bacteria is directly linked to cognitive problems in Alzheimer’s patients.
In Alzheimer's patients, there was a notable decrease in bacteria from the Coprococcus genus, which is linked to healthy ageing. Additionally, they had a higher presence of bacteria from the Desulfovibrio genus compared to cognitively healthy individuals, aligning with previous findings in animal models of Alzheimer's and Parkinson's disease.
These findings suggest that the gut microbiota plays a causative role in the development of Alzheimer’s symptoms, possibly revealing a novel way of treating and preventing the disease.
The research team also suggests that impaired neurogenesis could be the key connection between the changes in gut microbiota composition and cognitive decline in Alzheimer's disease.
Diet and alzheimer's
Some researchers have posited that diet plays a crucial role in the development of Alzheimer’s.
One recent review expands upon a previous hypothesis that links a survival mechanism that is stimulated by fructose consumption. Fructose is a type of sugar that, when eaten, induces insulin resistance which in turn helps preserve glucose for the brain.
Early features of Alzheimer’s include reduced cerebral glucose metabolism, mitochondrial dysfunction, and neuroinflammation, which could all be caused by diets high in sugar, high-glycemic carbohydrates, and salt.

Recent evidence has also demonstrated that having type 2 diabetes significantly increases the risk of Alzheimer's.
The two common diseases share several metabolic dysfunctions, such as insulin resistance, impaired glucose metabolism, and mitochondrial defects.
A ketogenic diet (which features little no sugar and carbohydrates) could be a useful intervention in treating and preventing both type 2 diabetes and Alzheimer’s.
Fungal cause?
In 2022, researchers at Baylor College of Medicine found that a common fungus called Candida albicans can enter the brain, triggering mechanisms similar to Alzheimer's disease.
The study found that Candida albicans, a fungus often found in the brains of people with Alzheimer’s disease, can break down the blood-brain barrier, causing damage in the brain, and generate amyloid beta-like peptides.
This research adds to growing evidence suggesting a link between infectious agents like fungi and neurodegenerative diseases.
Can Alzheimer’s be reversed?
Based on the above mentioned research, it’s clear that the cause of Alzheimer’s is not amyloid plaque build up - it’s only a symptom.
The true cause of the disease is likely a combination of environmental factors, including diet, toxins and stress, leading to insulin resistance, inflammation and mitochondrial dysfunction.
And there are many lifestyle interventions, supplements and off-patent drugs that can therefore help treat Alzheimer’s, possibly even reversing it.
Your doctor won’t promote these strategies much because the healthcare industry can’t profit from them.
However, there's plenty of evidence that middle-aged and older adults who focus on healthy habits like nutrition, exercise, social engagement and sleep can reduce their risk of Alzheimer’s, slow its onset, or even reverse its progression.

In 2014, Alzheimer’s researchers created a novel therapeutic program based on the underlying pathogenesis of Alzheimer's disease, such as insulin resistance, neuroinflammation and neurodegeneration (loss of brain cells).
The strategies include:
- Reducing carbohydrates and sugar to minimise inflammation and insulin resistance
- Promoting autophagy and ketogenesis through intermittent fasting
- Stress reduction techniques like mindful meditation
- Optimising sleep
- Engaging in regular exercise
- Maintaining vitamin D levels
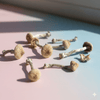
- Increasing Nerve Growth Factor (they used lion’s mane mushroom for this)
- Optimising antioxidant intake
- Addressing heavy metal toxicity
Nine of the 10 Alzheimer’s patients who undertook the program displayed an improvement in cognition after 6 months. The one failure being a patient in a very late stage of the disease.
Six of the patients had had to discontinue working or were struggling with their jobs at the beginning of the program, and all were able to return to work by the end.
Another study found the program effective at improving symptom scores of 100 Alzheimer’s patients, with many seeing an increase in hippocampal volume, the ability to spell returned, speech improved, and improvements in ability to shop, cook, and work at the computer.
Is Alzheimer’s genetic?
While genetics do play a role in Alzheimer's disease, it is a complex condition with multiple contributing factors.
The presence of specific genetic variants, particularly the APOE ε4 variant, can increase an individual's risk, but it does not guarantee the development of the disease.
Rather, the development of Alzheimer's is influenced by a combination of genetic, environmental, and lifestyle factors, and ongoing research is shedding light on its complexities.
Can lion’s mane mushroom help with Alzheimer’s?
There is some promising research that suggests that lion's mane mushroom may have potential benefits for individuals with Alzheimer's disease.
Compounds present in lion’s mane called hericenones and erinacines have been shown to promote the production of nerve growth factor (NGF), which plays a crucial role in the growth, maintenance, and survival of neurons in the brain.
By promoting the production of NGF and the growth of new brain cells, lion's mane mushroom may help protect against the degeneration of brain cells that occurs in Alzheimer's disease.

In 2020, researchers did a study to see if taking lion's mane mushroom supplements could help people with early Alzheimer's disease. The study lasted for one year and involved two groups of people, both of which had early Alzheimer's symptoms.
The results showed that the people who took the lion's mane supplements had better brain function compared to those who didn't take them. It also seemed like the mushroom supplement was safe and didn't cause any negative side effects for the Alzheimer's patients.
This study found that supplementation with lion's mane extract improved attention and cognitive function in individuals with mild cognitive impairment. Another found that consuming lion's mane prevents cognitive dysfunction in healthy adults.
In this study, researchers found that polysaccharides, which are a type of carbohydrate found in lion's mane mushroom, were able to reduce the damage caused to nerve cells by toxic chemicals that can harm the brain.
So while more research is needed to confirm these findings and to determine the optimal dosage, there is enough anecdotal and scientific research suggesting lion’s mane can help treat Alzheimer’s symptoms.
Learn more about lion’s mane here.
Conclusion
Alzheimer's is not down to the accumulation of amyloid plaques, but likely a combination of environmental factors, including diet, toxins, and stress, leading to insulin resistance, inflammation, and mitochondrial dysfunction.
Promisingly, lifestyle interventions, supplements, and off-patent drugs may offer potential treatments, and there is evidence that healthy habits like nutrition, exercise, social engagement, and sleep can reduce the risk, slow the onset, or even reverse the disease's progression.
Thanks to these new insights, there should be optimism about the future of Alzheimer’s treatment as we finally hone in on its actual causes.
Read: Can lion’s mane mushroom help with Alzheimer’s?
Sign up to our newsletter below for more Mushies magic 🍄🍄🍄